Insight

Adding to pharmacy’s case
In Insight
Bookmark
Record learning outcomes
It’s traditional to set out your stall in the run-up to contract negotiations, writes health economist Leela Barham. While the National Pharmacy Association doesn’t directly negotiate with the Government, it will want to influence the forthcoming negotiations on the national contract for England on behalf of its members.
Funding work from academics – in this case Professor David Taylor from University College London and Dr Panos Kanavos from the London School of Economics and Political Science – is part of the playbook, but what does it add?
Useful statistics
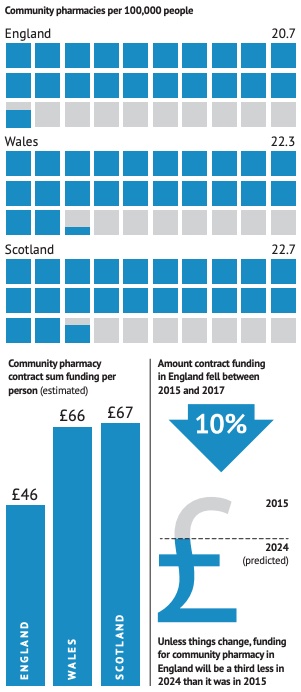
Protecting UK Public Interests in NHS Community Pharmacy has some new and useful stats for community pharmacy in England and how it compares to Wales and Scotland. Ministers generally dislike comparing badly to such close neighbours. Some highlights are set out in the diagram.
Learning from the neighbours
Much is made in the report of the differences across the UK when it comes to community pharmacy. There is an implicit criticism about a lack of joined-up policy on medicines in England and the UK more broadly, given how their use is shaped by many agencies, and with the concern that it would be unwise to have community pharmacists focus their efforts on unnecessary prescribing. Put very simply, community pharmacies can do so much more.
Taylor and Kanavos highlight good work in the devolved nations: Wales is focused on community pharmacy involvement in managing minor conditions, Pharmacy First in Scotland is cited as being more ambitious than efforts in England.
It’s not just what and how things are done, it matters too how the money is targeted. Funding is shifting in Wales, for example, with more money attached to services away from dispensing. Implicit is the advantage that the contract in Wales has clear financial incentives that are tied to the policy ambitions.
For balance, the authors also note how England is ahead when it comes to electronic prescribing, which could in turn enable internet pharmacy and hub and spoke dispensing. Despite the promise, these have been slow to get going in practice and haven’t yet brought hoped for efficiencies. They may not in any case, if the costs of the infrastructure are high and results in too few pharmacists being able to deliver more clinical services.
The message might be lost in the many paragraphs to get to it, but Taylor and Kanavos say that whatever the future holds when it comes to automated dispensing, there will still be a need for the pharmacist in person and not only that, but community pharmacy could do so much more. This, in turn, means adequate funding is needed.
£100 million retained margin doesn’t cut it
The authors are clear that even with the extra £100 million ‘over-payment’ for reimbursement being retained by community pharmacies in 2022 announced in September, it’s just not enough when pitched against the rising costs of running a pharmacy. There was already a strong narrative on this, but with inflation rising to 10 per cent, it’s become that bit more compelling. Taylor and Kanavos say that the risk of closures as a result is real.
Closing community pharmacies has an obvious and direct impact on those working there, but Taylor and Kanavos try to make the case that the ripple effect – disruption to NHS medicines supply and damage to the prospects for extended clinical services – is not in the public’s best interests.
The work is quiet, though, on just how much would be needed to keep those pharmacies alive, let alone thrive. £250m added to the global contract sum in 2023 and 2024 would only get the sector back to its 2015 level, according to Taylor and Kanavos. More is surely needed.
If it really is the case that the last commissioned work to look at inflation in community pharmacy dates from 2011 (by PwC), as Taylor and Kanavos suggest, then a detailed look that establishes baseline costs and how they are changing over time is long overdue.
Real costs and trends matter for pharmacies that are only just making ends meet, but who are delivering services that help patients while they do. Could the independent economic review commissioned by NHS England cover not only a new baseline, but also help give a more informed view of how costs are changing, to embed a reasonable growth rate into future funding?
Lack of informed scrutiny of policies
It could be easily missed, but the Taylor and Kanavos paper makes an important point about policy making and shaping. They suggest that policies that have led to big falls in real funding of community pharmacies in England have not been subject to “informed scrutiny beyond very limited circles”. That has resulted in policies that they suggest could have been rejected had they been “adequately understood.”
This is developed later in the report, with the assertion that community pharmacy in England has been shaped by the assumptions, capabilities and personal preferences of a small number of people. It’s easy to point out that this is not evidenced in the report – a lack of referencing is a picky, but justified, criticism across the piece – but it may well be true. It is certainly received wisdom across the sector.
That lays down a challenge for all those lobbying and representing community pharmacy in England to, in the simplest terms, ‘do better’ in future, not only in terms of having their eye on the ball, but also in opening up to new views and perspectives. There’s a risk that talking to the same people will simply end up with more of the same.
Taylor and Kanavos say that the ongoing UK Commission on Pharmacy Professional Leadership is welcome and will no doubt help. They also suggest that a parallel – and independent – effort could look at funding.
That could help too. But when it comes to the money, it’s both the Government and its agencies, as well as the Pharmaceutical Services Negotiating Committee, who need to take a good hard look at themselves and arguably do that much sooner than the commission and economic review will report.
No roadmap, unfortunately
The report summary ends: “With informed policy-making and goodwill, NHS community pharmacy could… evolve to become a clinical care and safe medicines supply profession in ways that will cost-effectively put modern patient and public interests first throughout the UK.”
That’s good as far as it goes, but it does little to provide a roadmap to achieving it. More money is an implicit call, but in the real world, more money will only come with strings attached – if it comes at all.
In fairness to Taylor and Kanavos, perhaps their brief never included the practical ‘what’s next’ question, but it’s something that needs to be answered. Because to properly protect the UK public interest in community pharmacy, the NPA and the sector as a whole have to think through new ways to be paid and to measure the value being delivered by community pharmacy. Fast.
For full disclosure, Leela Barham has worked with David Taylor in the past, but not on community pharmacy issues.

